ELECTRONIC POSTER - ismrm
ELECTRONIC POSTER - ismrm
ELECTRONIC POSTER - ismrm
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
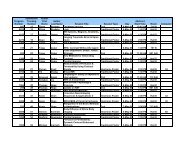
Wednesday 13:30-15:30 Computer 105<br />
13:30 4780. Relative Conspicuity of Prostate Cancer: Apparent Diffusion Coefficient Versus<br />
Dynamic Contrast Enhancement<br />
Daniel Jason Aaron Margolis 1 , Timothy McClure 1 , Steven Raman 1<br />
1 Department of Radiological Sciences, David Geffen School of Medicine at UCLA, Los Angeles, CA, United<br />
States<br />
Diffusion-weighted imaging (DWI) and dynamic contrast enhancement (DCE) can localize prostate cancer in situ, but it is unclear if<br />
one is superior. DWI, Ktrans, Kep, Ve, and T2WI are compared with surgical pathology in 23 patients using a unitless variable, the<br />
conspicuity ratio, the difference of the values from the ROI of the lesion and the contralateral side, divided by the average of these<br />
values. Prostate cancer is more conspicuous on DWI ADC maps and on DCE than on T2WI, and more conspicuous on DCE than on<br />
ADC, but Ktrans and Kep are not significantly different in terms of conspicuity.<br />
14:00 4781. Intersequence Variability in Multiparametric-Derived 3D Prostate Tumor<br />
Volumetrics at 3.0T<br />
Fiona M. Fennessy 1 , Sota Oguro 1 , Yi Tang 1 , Robert V. Mulkern 1 , Steven Haker 1 , Ehud J.<br />
Schmidt 1 , Sandeep Gupta 2 , Clare M. Tempany 1<br />
1 Radiology, Brigham and Women's Hospital, Boston, MA, United States; 2 GE Global Research, Niskayuna,,<br />
NY, United States<br />
Newer approaches for prostate cancer treatment mandate improvements in MR imaging to allow for accurate index lesion detection<br />
and display, to guide biopsy and focal therapy. In 9 pathology-proven prostate cancer patients, we manually segmented tumor<br />
according to multiparametric MR (mpMR) sequences using 3D-slicer software, and obtained volumetrics for each. Volumes based on<br />
DCE maps were significantly greater than those based on ADC maps (p=0.011) or T2WI (p=0.001), possibly reflecting different<br />
physiological properties of tumor assessed with mpMR. Volume discrepancies can be displayed in a single framework, and should be<br />
taken into consideration for tumor mapping in focal therapy planning.<br />
14:30 4782. The Utility of Prostate MRI Using Diffusion and Dynamic Enhanced Imaging in the<br />
Evaluation of Patients Previously Biopsy Negative for Cancer<br />
Andrew Dean Hardie 1<br />
1 Radiology, Medical University of South Carolina, Charleston, SC, United States<br />
Patients with an initial set of prostate biopsies which were negative for cancer were assessed by phased array MRI. All patients<br />
subsequently had repeat prostate biopsy which was used as the gold standard. The diagnostic accuracy of MRI, negative predictive<br />
value, and the difference in the number of biopsy samples performed in patients with cancer suspected by MRI and those unlikely to<br />
have cancer by MRI were assessed. MRI was 100% sensitive, 91% specific, and had a 100% negative predictive value for cancer.<br />
Less biopsy passes were performed in patients with an MRI read as likely to have cancer than those unlikely to have cancer by MRI.<br />
15:00 4783. Multiparametric Prostate MR Imaging and Spectroscopy in Patients with High-<br />
Risk Localized Prostate Cancer Before Radical Prostatectomy Assesses Risk of Extracapsular<br />
Extension And/or Positive Margins.<br />
Ernesto Castillo 1,2 , Emilio Hernandez 3 , Jose Maria Rodriguez-Barbero 4 , Pilar Perez<br />
Sanz 1 , Javier Gonzalez 3 , Pedro Cabrera 3 , Javier C. Angulo, 23<br />
1 Radiology, H.U. de Getafe, Getafe, Madrid, Spain; 2 Universidad Europea de Madrid; 3 Urology, H.U. de<br />
Getafe; 4 Pathology, H.U. de Getafe<br />
In 30 patients with high-risk localized (T1-2) prostate cancer the risk of extracapsular extension and affected margins before radical<br />
prostatectomy were evaluated blindly before surgery. The pathologists’ evaluation of the biopsy cylinders predicted the risk<br />
erroneously in 35% of the evaluations. Using multiparametric MRI and MR spectroscopic imaging, diffusion-weighted imaging and<br />
dynamic CE-MRI with an endorectal coil the radiologist did so in 18.3%. Multiparametric MRI of the prostate preoperatively alerts<br />
upon the risk of extracapsular disease in high-risk localized prostate cancer better than accurate review of transrectal biopsy.<br />
Thursday 13:30-15:30 Computer 105<br />
13:30 4784. MR-US Fusion for Targeted Prostate Biopsy<br />
Clifford Weiss 1 , Michael Seitz 2 , Karin Herrmann 3 , Arno Graser 3 , Berthold Kiefer 4 ,<br />
Martin Requardt 4 , Jens Fehre 4 , Ralf Nanke 4 , Mamadou Diallo 5 , Parmeshwar Khurd 5 , Ali<br />
Kamen 5 , Wolfgang Wein 5<br />
1 Center Department of Radiology, The Johns Hopkins University School of Medicine, Baltimore, MD, United<br />
States; 2 Urology Department, Ludwig Maximilian Universität München, München, Germany; 3 Radiology<br />
Department, Ludwig Maximilian Universität München, München, Germany; 4 Siemens Healthcare, Erlangen,<br />
Germany; 5 Imaging & Visualization Department, Siemens Corporate Research, Princeton, NJ, United States<br />
We aim to improve prostate targeted biopsy procedures, by taking pre-acquired diagnostic MRI images, and actively fusing them to<br />
the real-time trans-rectal ultrasound. In this way the diagnostic power of prostate MRI is married to the flexible, rapid and inexpensive<br />
ultrasound guided procedure. We propose a system based on a magnetically tracked freehand ultrasound probe, combined with a novel<br />
powerful deformable registration workflow that effectively compensates prostate organ deformation between the two modalities. We