- Page 1 and 2:
Review of Pharmacology Ninth Editio
- Page 3 and 4:
Dedicated to My parents, wife Prave
- Page 5 and 6:
Preface to the Ninth Edition We wan
- Page 7 and 8:
Acknowledgments When emotions are p
- Page 9 and 10:
References • Harrison’s Princip
- Page 11 and 12:
Contents 1. History of Pharmacology
- Page 13 and 14:
CHAPTER 1 History of pharmacology S
- Page 15 and 16:
CHAPTER 2 General Pharmacology Phar
- Page 17 and 18:
General Pharmacology Note: It is si
- Page 19 and 20:
General Pharmacology Drug metaboliz
- Page 21 and 22:
General Pharmacology Order of kinet
- Page 23 and 24:
General Pharmacology Therapeutic Dr
- Page 25 and 26:
General Pharmacology Fig. 2.4: G-pr
- Page 27 and 28:
General Pharmacology sigmoid shaped
- Page 29 and 30:
General Pharmacology Phase 1: Here,
- Page 31 and 32:
General Pharmacology 5. Essential m
- Page 33 and 34:
General Pharmacology (b) Bioavailab
- Page 35 and 36:
General Pharmacology (c) Are highly
- Page 37 and 38:
General Pharmacology (c) Strong aci
- Page 39 and 40:
General Pharmacology (a) 50 mg/hour
- Page 41 and 42:
General Pharmacology 140. Phamacoge
- Page 43 and 44:
General Pharmacology (c) Piroxicam
- Page 45 and 46:
206. Which of the following drugs s
- Page 47 and 48:
General Pharmacology 29. In which t
- Page 49 and 50:
General Pharmacology Explanations 1
- Page 51 and 52:
General Pharmacology • Other fact
- Page 53 and 54:
General Pharmacology -- Suppose, 10
- Page 55 and 56:
General Pharmacology 77. Ans. (a) W
- Page 57 and 58:
= 40 L × 4 mg/L = 160 mg Clearance
- Page 59 and 60:
General Pharmacology 126. Ans. (c)
- Page 61 and 62:
General Pharmacology 154. Ans. (d)
- Page 63 and 64:
General Pharmacology Intolerance is
- Page 65 and 66:
General Pharmacology 6. Ans. (b) b
- Page 67 and 68:
CHAPTER 3 Autonomic Nervous System
- Page 69 and 70:
Autonomic Nervous System Functions
- Page 71 and 72:
Autonomic Nervous System • Carbac
- Page 73 and 74:
Autonomic Nervous System used for g
- Page 75 and 76:
Autonomic Nervous System -- Central
- Page 77 and 78:
Autonomic Nervous System • Theref
- Page 79 and 80:
Autonomic Nervous System • Eye: S
- Page 81 and 82:
Autonomic Nervous System • Dopami
- Page 83 and 84:
Autonomic Nervous System • Phenox
- Page 85 and 86:
Autonomic Nervous System Lipid Inso
- Page 87 and 88:
Autonomic Nervous System Drug of Ch
- Page 89 and 90:
Multiple Choice Questions Autonomic
- Page 91 and 92:
Autonomic Nervous System (c) Organo
- Page 93 and 94:
(c) Physostigmime (d) Hyoscine hydr
- Page 95 and 96:
Autonomic Nervous System (c) Tropic
- Page 97 and 98:
132. A drug that blocks the uptake
- Page 99 and 100:
165. Clonidine is used for: (Kolkat
- Page 101 and 102:
as an effective substitute which do
- Page 103 and 104:
Autonomic Nervous System 13. Which
- Page 105 and 106:
Autonomic Nervous System (c) Increa
- Page 107 and 108:
Autonomic Nervous System 9. Ans. (a
- Page 109 and 110:
Autonomic Nervous System 39. Ans. (
- Page 111 and 112:
Autonomic Nervous System - Temazepa
- Page 113 and 114:
Autonomic Nervous System 103. Ans.
- Page 115 and 116:
Autonomic Nervous System have no ef
- Page 117 and 118:
Autonomic Nervous System 166. Ans.
- Page 119 and 120:
Autonomic Nervous System 194. Ans.
- Page 121 and 122:
Autonomic Nervous System 23. Ans. (
- Page 123 and 124:
CHAPTER 4 Autacoids These are the s
- Page 125 and 126:
Autacoids All second generation ant
- Page 127 and 128:
Autacoids v v v v v Calcium channel
- Page 129 and 130:
Autacoids nary bypass. It can also
- Page 131 and 132:
Autacoids to presence of sulfur con
- Page 133 and 134:
Autacoids Rheumatoid Arthritis Rheu
- Page 135 and 136:
Autacoids It is a monoclonal antibo
- Page 137 and 138:
Autacoids Drug of choice Condition
- Page 139 and 140:
15. Anti-vertigo drug which modulat
- Page 141 and 142:
49. Sumatriptan is: (DPG 1999, TN 2
- Page 143 and 144:
81. All of the following effects ar
- Page 145 and 146:
114. Which prostaglandin helps in c
- Page 147 and 148:
Autacoids 148. Which of the followi
- Page 149 and 150:
Autacoids 30. A 15 year old boy was
- Page 151 and 152:
Autacoids 16. Ans. (b) Dangerous ve
- Page 153 and 154:
Autacoids 56. Ans. (c) Cyclooxygena
- Page 155 and 156:
Autacoids 85. Ans. (b) Aspirin supp
- Page 157 and 158:
Autacoids 125. Ans. (b) Indomethaci
- Page 159 and 160:
Autacoids 13. Ans. (a) Naproxen (Re
- Page 161 and 162:
CHAPTER 5 Cardiovascular System CON
- Page 163 and 164:
Cardiovascular System In atrial fib
- Page 165 and 166:
Cardiovascular System Treatment of
- Page 167 and 168:
Cardiovascular System should be use
- Page 169 and 170:
Cardiovascular System tive α 1 blo
- Page 171 and 172:
Cardiovascular System nifedipine an
- Page 173 and 174:
Cardiovascular System Treatment of
- Page 175 and 176:
Cardiovascular System ANGINA PECTOR
- Page 177 and 178:
Cardiovascular System BETA BLOCKERS
- Page 179 and 180:
Cardiovascular System The action po
- Page 181 and 182:
Cardiovascular System depolarized c
- Page 183 and 184:
Cardiovascular System • Digoxin i
- Page 185 and 186:
Cardiovascular System Contd... •
- Page 187 and 188:
Cardiovascular System DRUG OF CHOIC
- Page 189 and 190:
15. Digoxin toxicity is aggravated
- Page 191 and 192:
(c) Treat digoxin toxicity (d) Rapi
- Page 193 and 194:
(c) Decreases sodium and increases
- Page 195 and 196:
Cardiovascular System 113. All of t
- Page 197 and 198:
146. Which of the following drugs i
- Page 199 and 200:
Cardiovascular System 180. Characte
- Page 201 and 202:
213. In a patient with hypertriglyc
- Page 203 and 204:
247. ACE inhibitors cause: (PGI Dec
- Page 205 and 206:
Cardiovascular System 16. Dialysis
- Page 207 and 208:
Cardiovascular System 53. Which of
- Page 209 and 210:
• Nesiritide is a recombinant BNP
- Page 211 and 212:
Cardiovascular System 43. Ans. (d)
- Page 213 and 214:
Cardiovascular System 81. Ans. (a)
- Page 215 and 216:
Cardiovascular System -- Hypertensi
- Page 217 and 218:
Cardiovascular System Cyanide has v
- Page 219 and 220:
Cardiovascular System 178. Ans. (a)
- Page 221 and 222:
Cardiovascular System 217. Ans. (a)
- Page 223 and 224:
Cardiovascular System 237. Ans. (a)
- Page 225 and 226:
Cardiovascular System 13. Ans (b) P
- Page 227 and 228:
CHAPTER 6 Kidney Diuretics Diuretic
- Page 229 and 230:
Kidney Uses Main use of loop diuret
- Page 231 and 232:
Kidney • Amiloride is more potent
- Page 233 and 234:
Kidney Amiloride It is the agent of
- Page 235 and 236:
Kidney Multiple Choice Questions di
- Page 237 and 238:
30. Which of the following statemen
- Page 239 and 240:
66. Advantage of desmopressin over
- Page 241 and 242:
Kidney Explanations 1. Ans. (b) Hyp
- Page 243 and 244:
16. Ans. (b) Bumetanide (Ref: KDT 6
- Page 245 and 246:
Kidney 55. Ans (d) V 4 : Central Ne
- Page 247 and 248:
CHAPTER 7 Endocrinology Hormones ar
- Page 249 and 250:
Endocrinology Prolactin It causes g
- Page 251 and 252:
Endocrinology • In the liver and
- Page 253 and 254:
Endocrinology I 131 can be used for
- Page 255 and 256:
Endocrinology Drug interactions •
- Page 257 and 258:
Endocrinology Lactic acidosis (more
- Page 259 and 260:
Endocrinology 3. amylin analogs Pra
- Page 261 and 262:
Endocrinology Important Points Maxi
- Page 263 and 264:
Endocrinology • Steroids with sel
- Page 265 and 266:
Endocrinology • Vitamin D 2 is er
- Page 267 and 268:
Endocrinology Denosumab Osteoclasts
- Page 269 and 270:
Endocrinology • SERMs are targete
- Page 271 and 272:
Endocrinology Contd... • Uliprist
- Page 273 and 274:
Endocrinology only pills. Chances o
- Page 275 and 276:
Endocrinology Pharmacokinetics Test
- Page 277 and 278:
Endocrinology Ergot Derivatives Erg
- Page 279 and 280:
Endocrinology Contd... • Hyperpro
- Page 281 and 282:
completion of therapy, the patient
- Page 283 and 284:
(c) Glucose (d) Starch 47. True abo
- Page 285 and 286:
(c) Na + exit/K + entry (d) K + ent
- Page 287 and 288:
Endocrinology 113. Which of the fol
- Page 289 and 290:
147. Bisphosphonates act by: (AI 20
- Page 291 and 292:
180. Women receiving estrogen thera
- Page 293 and 294:
(c) Clomiphene (d) Mifepristone (RU
- Page 295 and 296:
246. Mechanism of Calcitriol is: (R
- Page 297 and 298:
Endocrinology 32. Drug used to cont
- Page 299 and 300:
(b) Glimepiride (c) Repaglinide (d)
- Page 301 and 302:
Endocrinology Explanations 1. Ans.
- Page 303 and 304:
Endocrinology 24. Ans. (c) Propylth
- Page 305 and 306:
Endocrinology • When this drug is
- Page 307 and 308:
Endocrinology Hypoglycemia is cause
- Page 309 and 310:
Endocrinology Drugs causing Addison
- Page 311 and 312:
Endocrinology Raloxifene is a selec
- Page 313 and 314:
Endocrinology • Enzyme inducers l
- Page 315 and 316:
Endocrinology 197. Ans. (b) Blocks
- Page 317 and 318:
Endocrinology A spider angioma (als
- Page 319 and 320:
Endocrinology 4. Ans (c) Glaucoma (
- Page 321 and 322:
Endocrinology 70. Ans. (c) Mifepris
- Page 323 and 324:
NOTES _____________________________
- Page 325 and 326:
CHAPTER 8 Central Nervous System Se
- Page 327 and 328:
Central Nervous System It is admini
- Page 329 and 330:
Central Nervous System • Abnormal
- Page 331 and 332:
Central Nervous System useful in AD
- Page 333 and 334:
Central Nervous System Wilson’s D
- Page 335 and 336:
Central Nervous System Important Dr
- Page 337 and 338:
Central Nervous System • Lamotrig
- Page 339 and 340:
Central Nervous System play a role
- Page 341 and 342:
Central Nervous System According to
- Page 343 and 344:
Central Nervous System bulimia, pre
- Page 345 and 346:
Central Nervous System Anti Manic D
- Page 347 and 348:
Central Nervous System dependence,
- Page 349 and 350:
Central Nervous System increase hea
- Page 351 and 352:
Central Nervous System Actions •
- Page 353 and 354:
Central Nervous System Contd... •
- Page 355 and 356:
(c) Alkalization of the urine will
- Page 357 and 358:
Central Nervous System (c) Ketamine
- Page 359 and 360:
79. Drug of choice for myoclonic ep
- Page 361 and 362:
(c) Phenytoin (d) Valproic acid 112
- Page 363 and 364:
146. Which of the following antipsy
- Page 365 and 366:
(c) Regular measurements of blood c
- Page 367 and 368:
210. A patient Rajnish having depre
- Page 369 and 370:
242. Drug useful in malignant hyper
- Page 371 and 372:
279. Preferred drug for alcohol wit
- Page 373 and 374:
314. Morphine can administered by a
- Page 375 and 376:
(c) Analgesia (d) Mydriasis 348. Di
- Page 377 and 378:
17. Antiparkinson drug known to cau
- Page 379 and 380:
53. Which drug is the most useful i
- Page 381 and 382:
Central Nervous System 15. Ans. (c)
- Page 383 and 384:
Central Nervous System 39. Ans. (b)
- Page 385 and 386:
67. Ans. (a) Phenytoin (Ref: Katzun
- Page 387 and 388:
97. Ans. (a) Hepatitis (Ref: KDT 6/
- Page 389 and 390:
Central Nervous System 145. Ans (c)
- Page 391 and 392:
Central Nervous System 159. Ans. (d
- Page 393 and 394:
Central Nervous System 187. Ans. (b
- Page 395 and 396:
Central Nervous System 212. Ans. (a
- Page 397 and 398:
Central Nervous System 258. Ans. (a
- Page 399 and 400:
Central Nervous System 286. Ans. (b
- Page 401 and 402:
Central Nervous System 303. Ans. (c
- Page 403 and 404:
Central Nervous System 326. Ans. (c
- Page 405 and 406:
Central Nervous System 366. Ans. (b
- Page 407 and 408:
Central Nervous System 60. Ans. (a)
- Page 409 and 410:
CHAPTER 9 Anaesthesia Local Anaesth
- Page 411 and 412:
Anaesthesia trigeminal nerve, cervi
- Page 413 and 414:
Anaesthesia Centrally Acting Muscle
- Page 415 and 416:
Anaesthesia • These drugs release
- Page 417 and 418:
Anaesthesia Anaesthetic MAC (% atm)
- Page 419 and 420:
Anaesthesia Methemoglobinemia and l
- Page 421 and 422:
Anaesthesia Chloroform • It is a
- Page 423 and 424:
Anaesthesia Contd... • It does no
- Page 425 and 426:
Anaesthesia Anaesthetic agents of c
- Page 427 and 428:
Anaesthesia Multiple Choice Questio
- Page 429 and 430:
33. Post dural (Spinal) puncture he
- Page 431 and 432:
(b) Dantrolene (c) Succinylcholine
- Page 433 and 434:
103. Which of the following drugs a
- Page 435 and 436:
Anaesthesia 138. Thiopental sodium
- Page 437 and 438:
Anaesthesia Explanations 1. Ans (c)
- Page 439 and 440:
Anaesthesia 20. Ans. (d) Seizures a
- Page 441 and 442:
Anaesthesia 49. Ans. (b) Meprobamat
- Page 443 and 444:
Anaesthesia • The patient underwe
- Page 445 and 446:
Anaesthesia 91. Ans. (b) Sevofluran
- Page 447 and 448:
Anaesthesia • In pheochromocytoma
- Page 449 and 450:
CHAPTER 10 Hematology HAEMATINICS T
- Page 451 and 452:
Hematology • Deficiency of folic
- Page 453 and 454:
Hematology • Main drugs acting as
- Page 455 and 456:
Hematology 1. Oral Anticoagulants
- Page 457 and 458:
Hematology • Bioavailability of u
- Page 459 and 460:
Hematology • Rodenticides contain
- Page 461 and 462:
Hematology Condition • Anemia Dru
- Page 463 and 464:
(c) Erythropoietin (d) Filgrastim (
- Page 465 and 466:
Hematology 46. Tirofiban is a: (RJ
- Page 467 and 468:
80. The anticoagulant of choice in
- Page 469 and 470:
6. Mechanism of action of clopidogr
- Page 471 and 472: Hematology Explanations 1. Ans. (c)
- Page 473 and 474: Hematology 17. Ans. (d) Oprelvekin
- Page 475 and 476: Hematology 51. Ans. (a) Dabigatran:
- Page 477 and 478: Hematology 71. Ans. (c) Warfarin (R
- Page 479 and 480: Hematology 106. Ans. (c) Streptokin
- Page 481 and 482: CHAPTER 11 Respiratory System Cough
- Page 483 and 484: Respiratory System fast acting also
- Page 485 and 486: Respiratory System LT receptor anta
- Page 487 and 488: Respiratory System Condition • Br
- Page 489 and 490: 17. The most prominent and dose rel
- Page 491 and 492: Respiratory System 52. In theophyll
- Page 493 and 494: Respiratory System Explanations 1.
- Page 495 and 496: Respiratory System • Inhalational
- Page 497 and 498: CHAPTER 12 Gastrointestinal Tract P
- Page 499 and 500: Gastrointestinal Tract Contd... --
- Page 501 and 502: Gastrointestinal Tract Anti Emetic
- Page 503 and 504: Gastrointestinal Tract Domperidone
- Page 505 and 506: Gastrointestinal Tract Oral Rehydra
- Page 507 and 508: Gastrointestinal Tract Condition
- Page 509 and 510: (c) Misoprostol (d) Omeprazole 15.
- Page 511 and 512: 49. The most effective antiemetic f
- Page 513 and 514: Gastrointestinal Tract recent Quest
- Page 515 and 516: Gastrointestinal Tract Explanations
- Page 517 and 518: Gastrointestinal Tract 30. Ans. (b)
- Page 519 and 520: Gastrointestinal Tract 1. EarlyPhas
- Page 521: Gastrointestinal Tract 17. Ans. (c)
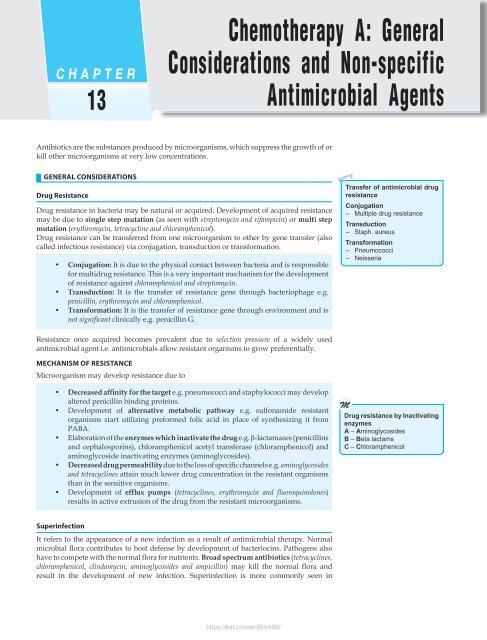
- Page 525 and 526: Chemotherapy A: General Considerati
- Page 527 and 528: contd... Drugs Binds to Mechanism o
- Page 529 and 530: Chemotherapy A: General Considerati
- Page 531 and 532: Chemotherapy A: General Considerati
- Page 533 and 534: Contd... Chemotherapy A: General Co
- Page 535 and 536: Chemotherapy A: General Considerati
- Page 537 and 538: Clinical Uses Chemotherapy A: Gener
- Page 539 and 540: Chemotherapy A: General Considerati
- Page 541 and 542: Chemotherapy A: General Considerati
- Page 543 and 544: Chemotherapy A: General Considerati
- Page 545 and 546: Important Points About Antimicrobia
- Page 547 and 548: Chemotherapy A: General Considerati
- Page 549 and 550: Chemotherapy A: General Considerati
- Page 551 and 552: Chemotherapy A: General Considerati
- Page 553 and 554: Chemotherapy A: General Considerati
- Page 555 and 556: Chemotherapy A: General Considerati
- Page 557 and 558: Chemotherapy A: General Considerati
- Page 559 and 560: Chemotherapy A: General Considerati
- Page 561 and 562: Chemotherapy A: General Considerati
- Page 563 and 564: Chemotherapy A: General Considerati
- Page 565 and 566: Chemotherapy A: General Considerati
- Page 567 and 568: Chemotherapy A: General Considerati
- Page 569 and 570: Chemotherapy A: General Considerati
- Page 571 and 572: Chemotherapy A: General Considerati
- Page 573 and 574:
Chemotherapy A: General Considerati
- Page 575 and 576:
Chemotherapy A: General Considerati
- Page 577 and 578:
Chemotherapy A: General Considerati
- Page 579 and 580:
128. Ans. (b) Trovafloxacin (Goodma
- Page 581 and 582:
Chemotherapy A: General Considerati
- Page 583 and 584:
Chemotherapy A: General Considerati
- Page 585 and 586:
Chemotherapy A: General Considerati
- Page 587 and 588:
Chemotherapy A: General Considerati
- Page 589 and 590:
CHAPTER 14 Chemotherapy B: Antimicr
- Page 591 and 592:
Chemotherapy B: Antimicrobials for
- Page 593 and 594:
Clofazimine It is a dye with lepros
- Page 595 and 596:
Chemotherapy B: Antimicrobials for
- Page 597 and 598:
Foscarnet It is not an antimetaboli
- Page 599 and 600:
Human Immunodeficiency Virus (HIV)
- Page 601 and 602:
Chemotherapy B: Antimicrobials for
- Page 603 and 604:
Chemotherapy B: Antimicrobials for
- Page 605 and 606:
Chemotherapy B: Antimicrobials for
- Page 607 and 608:
Chemotherapy B: Antimicrobials for
- Page 609 and 610:
Chemotherapy B: Antimicrobials for
- Page 611 and 612:
Chemotherapy B: Antimicrobials for
- Page 613 and 614:
Chemotherapy B: Antimicrobials for
- Page 615 and 616:
16. Bactericidal drugs in ATT are:
- Page 617 and 618:
50. Ethambutol should be used very
- Page 619 and 620:
Chemotherapy B: Antimicrobials for
- Page 621 and 622:
120. Regarding ritonavir use in AID
- Page 623 and 624:
ACTs). All of the following combina
- Page 625 and 626:
Chemotherapy B: Antimicrobials for
- Page 627 and 628:
ecent Questions asked by National B
- Page 629 and 630:
Chemotherapy B: Antimicrobials for
- Page 631 and 632:
Explanations Chemotherapy B: Antimi
- Page 633 and 634:
25. Ans. (b) Ethionamide (Ref: KDT
- Page 635 and 636:
Chemotherapy B: Antimicrobials for
- Page 637 and 638:
Chemotherapy B: Antimicrobials for
- Page 639 and 640:
Chemotherapy B: Antimicrobials for
- Page 641 and 642:
Chemotherapy B: Antimicrobials for
- Page 643 and 644:
Chemotherapy B: Antimicrobials for
- Page 645 and 646:
Chemotherapy B: Antimicrobials for
- Page 647 and 648:
CHAPTER 15 Chemotherapy C: Antineop
- Page 649 and 650:
Chemotherapy C: Antineoplastic Drug
- Page 651 and 652:
Chemotherapy C: Antineoplastic Drug
- Page 653 and 654:
4-5 years). Another distinguishing
- Page 655 and 656:
Chemotherapy C: Antineoplastic Drug
- Page 657 and 658:
GnRH Antagonists Cetrorelix, ganire
- Page 659 and 660:
This drug was used in 1960s as a se
- Page 661 and 662:
Chemotherapy C: Antineoplastic Drug
- Page 663 and 664:
Multiple Choice Questions Chemother
- Page 665 and 666:
37. Which of the following statemen
- Page 667 and 668:
Chemotherapy C: Antineoplastic Drug
- Page 669 and 670:
Chemotherapy C: Antineoplastic Drug
- Page 671 and 672:
Chemotherapy C: Antineoplastic Drug
- Page 673 and 674:
Chemotherapy C: Antineoplastic Drug
- Page 675 and 676:
Chemotherapy C: Antineoplastic Drug
- Page 677 and 678:
Chemotherapy C: Antineoplastic Drug
- Page 679 and 680:
Chemotherapy C: Antineoplastic Drug
- Page 681 and 682:
Chemotherapy C: Antineoplastic Drug
- Page 683 and 684:
Chemotherapy C: Antineoplastic Drug
- Page 685 and 686:
CHAPTER 16 Immunomodulators IMMUNOS
- Page 687 and 688:
Immunomodulators 9. Antibodies Poly
- Page 689 and 690:
Immunomodulators Examples of each t
- Page 691 and 692:
Immunomodulators Clinical Diagnosis
- Page 693 and 694:
(b) Podophylline (c) Interferon (d)
- Page 695 and 696:
(c) Cytarabine (d) Cycloserine 51.
- Page 697 and 698:
Immunomodulators Explanations 1. An
- Page 699 and 700:
Immunomodulators 14. Ans. (a) Syste
- Page 701 and 702:
Immunomodulators 33. Ans. (a) Gluco
- Page 703 and 704:
CHAPTER 17 Other Topics and Adverse
- Page 705 and 706:
Other Topics and Adverse Effects Co
- Page 707 and 708:
Other Topics and Adverse Effects Co
- Page 709 and 710:
Other Topics and Adverse Effects Co
- Page 711 and 712:
17. A 2 years old child without fev
- Page 713 and 714:
54. Isotretinoin is: (PGI June, 200
- Page 715 and 716:
Other Topics and Adverse Effects (c
- Page 717 and 718:
Other Topics and Adverse Effects
- Page 719 and 720:
Other Topics and Adverse Effects
- Page 721 and 722:
Other Topics and Adverse Effects 39
- Page 723 and 724:
Other Topics and Adverse Effects 55
- Page 725 and 726:
Other Topics and Adverse Effects Dr
- Page 727 and 728:
CHAPTER 18 Drugs of Choice Drug of
- Page 729 and 730:
Drugs of Choice Contd... Hypertensi
- Page 731 and 732:
Contd... VRSA LINEZOLID/STREPTOGRAM
- Page 733 and 734:
CHAPTER 19 New Drugs 1. Abatacept:
- Page 735 and 736:
New Drugs 52. Canakinumab: A human
- Page 737 and 738:
New Drugs 100. Ecallantide: A plasm
- Page 739 and 740:
New Drugs 153. Laronidase: Recombin
- Page 741 and 742:
New Drugs 204. Peginesatide: A pept
- Page 743 and 744:
New Drugs been approved for the tre
- Page 745 and 746:
New Drugs and B lymphocytes after e
- Page 747 and 748:
New Drugs prevents nausea and vomit
- Page 749 and 750:
CHAPTER 20 Recent Topics TRICYCLIC
- Page 751 and 752:
Recent Topics 2. Drugs 5-HT 2 recep
- Page 753 and 754:
Recent Topics Arginine NOS NO + Cit
- Page 755 and 756:
Recent Topics Contd... Drug Tetracy
- Page 757 and 758:
Recent Topics -- If the patient has
- Page 759 and 760:
CHAPTER 21 Latest Papers AIIMS Nove
- Page 761 and 762:
Latest Papers explanations 1. Ans.
- Page 763 and 764:
• Clindamycin and erythromycin ar
- Page 765 and 766:
Latest Papers AIIMS May 2014 1. Whi
- Page 767 and 768:
Latest Papers explanations 1. Ans.
- Page 769 and 770:
13. Ans. a. Hypokalemia (Ref: Harri
- Page 771 and 772:
NOTES _____________________________
- Page 773 and 774:
Image Based Questions https://kat.c
- Page 775 and 776:
Image Based Questions 1. The result
- Page 777 and 778:
5. A new antiarrhythmic drug is fou
- Page 779 and 780:
10. Amarnath, a 58 year old busines
- Page 781 and 782:
14. A 72-year-old male, Hemraj was
- Page 783 and 784:
(rapid vs slow induction of anesthe