ÐбÑÑник Ñез XVI ÐÑжнаÑодно медиÑного конгÑеÑÑ ÑÑÑденÑÑв Ñа ...
ÐбÑÑник Ñез XVI ÐÑжнаÑодно медиÑного конгÑеÑÑ ÑÑÑденÑÑв Ñа ...
ÐбÑÑник Ñез XVI ÐÑжнаÑодно медиÑного конгÑеÑÑ ÑÑÑденÑÑв Ñа ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
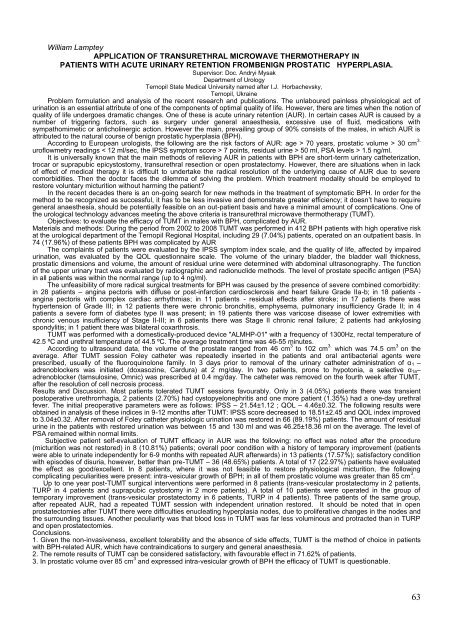
William Lamptey<br />
APPLICATION OF TRANSURETHRAL MICROWAVE THERMOTHERAPY IN<br />
PATIENTS WITH ACUTE URINARY RETENTION FROMBENIGN PROSTATIC HYPERPLASIA.<br />
Supervisor: Doc. Andryi Mysak<br />
Department of Urology<br />
Ternopil State Medical University named after I.J. Horbachevsky,<br />
Ternopil, Ukraine<br />
Problem formulation and analysis of the recent research and publications. The unlaboured painless physiological act of<br />
urination is an essential attribute of one of the components of optimal quality of life. However, there are times when the notion of<br />
quality of life undergoes dramatic changes. One of these is acute urinary retention (AUR). In certain cases AUR is caused by a<br />
number of triggering factors, such as surgery under general anaesthesia, excessive use of fluid, medications with<br />
sympathomimetic or anticholinergic action. However the main, prevailing group of 90% consists of the males, in which AUR is<br />
attributed to the natural course of benign prostatic hyperplasia (BPH).<br />
According to European urologists, the following are the risk factors of AUR: age > 70 years, prostatic volume > 30 cm 3.<br />
uroflowmetry readings < 12 ml/sec, the ІPSS symptom score > 7 points, residual urine > 50 ml, PSA levels > 1.5 ng/ml.<br />
It is universally known that the main methods of relieving AUR in patients with BPH are short-term urinary catheterization,<br />
trocar or suprapubic epicystostomy, transurethral resection or open prostatectomy. However, there are situations when in lack<br />
of effect of medical therapy it is difficult to undertake the radical resolution of the underlying cause of AUR due to severe<br />
comorbidities. Then the doctor faces the dilemma of solving the problem. Which treatment modality should be employed to<br />
restore voluntary micturition without harming the patient<br />
In the recent decades there is an on-going search for new methods in the treatment of symptomatic BPH. In order for the<br />
method to be recognized as successful, it has to be less invasive and demonstrate greater efficiency; it doesn‘t have to require<br />
general anaesthesia, should be potentially feasible on an out-patient basis and have a minimal amount of complications. One of<br />
the urological technology advances meeting the above criteria is transurethral microwave thermotherapy (TUMT).<br />
Objectives: to evaluate the efficacy of TUMT in males with BPH, complicated by AUR.<br />
Materials and methods: During the period from 2002 to 2008 TUMT was performed in 412 BPH patients with high operative risk<br />
at the urological department of the Ternopil Regional Hospital, including 29 (7.04%) patients, operated on an outpatient basis. In<br />
74 (17.96%) of these patients BPH was complicated by AUR<br />
The complaints of patients were evaluated by the IPSS symptom index scale, and the quality of life, affected by impaired<br />
urination, was evaluated by the QOL questionnaire scale. The volume of the urinary bladder, the bladder wall thickness,<br />
prostatic dimensions and volume, the amount of residual urine were determined with abdominal ultrasonography. The function<br />
of the upper urinary tract was evaluated by radiographic and radionuclide methods. The level of prostate specific antigen (PSA)<br />
in all patients was within the normal range (up to 4 ng/ml).<br />
The unfeasibility of more radical surgical treatments for BPH was caused by the presence of severe combined comorbidity:<br />
in 28 patients – angina pectoris with diffuse or post-infarction cardiosclerosis and heart failure Grade IIa-b; in 18 patients -<br />
angina pectoris with complex cardiac arrhythmias; in 11 patients - residual effects after stroke; in 17 patients there was<br />
hypertension of Grade III; in 12 patients there were chronic bronchitis, emphysema, pulmonary insufficiency Grade II; in 4<br />
patients a severe form of diabetes type II was present; in 19 patients there was varicose disease of lower extremities with<br />
chronic venous insufficiency of Stage II-III; in 6 patients there was Stage II chronic renal failure; 2 patients had ankylosing<br />
spondylitis; in 1 patient there was bilateral coxarthrosis.<br />
TUMT was performed with a domestically-produced device "ALMHP-01" with a frequency of 1300Hz, rectal temperature of<br />
42.5 ºC and urethral temperature of 44.5 ºC. The average treatment time was 46-55 minutes.<br />
According to ultrasound data, the volume of the prostate ranged from 46 cm 3 to 102 cm 3. which was 74.5 cm 3 on the<br />
average. After TUMT session Foley catheter was repeatedly inserted in the patients and oral antibacterial agents were<br />
prescribed, usually of the fluoroquinolone family. In 3 days prior to removal of the urinary catheter administration of α 1 –<br />
adrenoblockers was initiated (doxasozine, Cardura) at 2 mg/day. In two patients, prone to hypotonia, a selective α 1а–<br />
adrenoblocker (tamsulosine, Omnic) was prescribed at 0.4 mg/day. The catheter was removed on the fourth week after TUMT,<br />
after the resolution of cell necrosis process.<br />
Results and Discussion. Most patients tolerated TUMT sessions favourably. Only in 3 (4.05%) patients there was transient<br />
postoperative urethrorrhagia, 2 patients (2.70%) had cystopyelonephritis and one more patient (1.35%) had a one-day urethral<br />
fever. The initial preoperative parameters were as follows: IPSS – 21.54±1.12 ; QOL – 4.46±0.32. The following results were<br />
obtained in analysis of these indices in 9-12 months after TUMT: IPSS score decreased to 18.51±2.45 and QOL index improved<br />
to 3.04±0.32. After removal of Foley catheter physiologic urination was restored in 66 (89.19%) patients. The amount of residual<br />
urine in the patients with restored urination was between 15 and 130 ml and was 46.25±18.36 ml on the average. The level of<br />
PSA remained within normal limits.<br />
Subjective patient self-evaluation of TUMT efficacy in AUR was the following: no effect was noted after the procedure<br />
(micturition was not restored) in 8 (10.81%) patients; overall poor condition with a history of temporary improvement (patients<br />
were able to urinate independently for 6-9 months with repeated AUR afterwards) in 13 patients (17.57%); satisfactory condition<br />
with episodes of disuria, however, better than pre-TUMT – 36 (48.65%) patients. A total of 17 (22.97%) patients have evaluated<br />
the effect as good/excellent. In 8 patients, where it was not feasible to restore physiological micturition, the following<br />
complicating peculiarities were present: intra-vesicular growth of BPH; in all of them prostatic volume was greater than 85 cm 3 .<br />
Up to one year post-TUMT surgical interventions were performed in 8 patients (trans-vesicular prostatectomy in 2 patients,<br />
TURP in 4 patients and suprapubic cystostomy in 2 more patients). A total of 10 patients were operated in the group of<br />
temporary improvement (trans-vesicular prostatectomy in 6 patients, TURP in 4 patients). Three patients of the same group,<br />
after repeated AUR, had a repeated TUMT session with independent urination restored. It should be noted that in open<br />
prostatectomies after TUMT there were difficulties enucleating hyperplasia nodes, due to proliferative changes in the nodes and<br />
the surrounding tissues. Another peculiarity was that blood loss in TUMT was far less voluminous and protracted than in TURP<br />
and open prostatectomies.<br />
Conclusions.<br />
1. Given the non-invasiveness, excellent tolerability and the absence of side effects, TUMT is the method of choice in patients<br />
with BPH-related AUR, which have contraindications to surgery and general anaesthesia.<br />
2. The remote results of TUMT can be considered satisfactory, with favourable effect in 71.62% of patients.<br />
3. In prostatic volume over 85 cm 3 and expressed intra-vesicular growth of BPH the efficacy of TUMT is questionable.<br />
63