- Page 1 and 2:
LIST OF CHAPTERS PART 2 - CLAIMS (I
- Page 3 and 4:
which may be useful to the CE. b. C
- Page 5 and 6:
d. Continuation of Pay. An employee
- Page 7 and 8:
o. Review of OWCP Decisions. Under
- Page 9 and 10:
2-0300 COMMUNICATIONS TABLE OF CONT
- Page 11 and 12:
2-0300-4 Regular Correspondence 4.R
- Page 13 and 14:
(b) Formal Decision. If a formal de
- Page 15 and 16:
If the information requested cannot
- Page 17 and 18:
eferred to the NOO for adjudication
- Page 19 and 20:
2-0400-6 Requesting Files 6. Reques
- Page 21 and 22:
the file. This process should mainl
- Page 23 and 24:
2-0400-10 Case Transfers and Loans
- Page 25 and 26:
2-0401 AUTOMATED SYSTEM SUPPORT FOR
- Page 27 and 28:
names and addresses is optional. By
- Page 29 and 30:
PW: Entitled to payment on periodic
- Page 31 and 32:
AM/C1: Condition accepted. Up to $1
- Page 33 and 34:
full appeal rights, and the adjudic
- Page 35 and 36:
B Both A Aggravation 2-0402 SECURIT
- Page 37 and 38:
a. Signatures. The CE must review c
- Page 39 and 40:
(a) The particular issues about whi
- Page 41 and 42:
c. Review by DD. Upon receipt of th
- Page 43 and 44:
disposition, a report, enclosing th
- Page 45 and 46:
2-0500 CONFERENCING TABLE OF CONTEN
- Page 47 and 48:
necessary to identify the official(
- Page 49 and 50:
2-0500-6 Senior CE Actions 6. Senio
- Page 51 and 52:
2-0500-9 Due Process 9. Due Process
- Page 53 and 54:
This chapter outlines the major ste
- Page 55 and 56:
(d) Been notified that OWCP will pr
- Page 57 and 58:
2-0600-4 Initial Actions 4. Initial
- Page 59 and 60:
2-0600-5 Nurse Services 5. Nurse Se
- Page 61 and 62:
assess the claimant's environment a
- Page 63 and 64:
(4) Timely responses to telephone c
- Page 65 and 66:
for guidance in composing such ques
- Page 67 and 68:
(4) Only if the CE has taken these
- Page 69 and 70:
(1) RS Actions. If the claimant agr
- Page 71 and 72:
(3) Absent such a recovery, the OWC
- Page 73 and 74:
(c) After any training or other pre
- Page 75 and 76:
under way and the CE determines tha
- Page 77 and 78:
2-0600 Exhibit 1: Sample Letter to
- Page 79 and 80:
2-0600 Exhibit 3: Example of Letter
- Page 81 and 82:
2-0600 Exhibit 5: Planning Chart fo
- Page 83 and 84:
period, and each new recurrence. a.
- Page 85 and 86:
a. QCM Screen. When the QCM screen
- Page 87 and 88:
(c) Confirmation of Data. After ent
- Page 89 and 90:
(1) NFN*--Referred to Field Nurse.
- Page 91 and 92:
2-0601-6 Effect of RTW on QCM Statu
- Page 93 and 94:
2-0601 Exhibit 1: Disability Tracki
- Page 95 and 96:
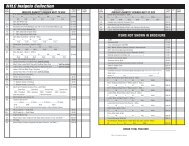
SRE Referred to SrCE for Conference
- Page 97 and 98:
21. FECA Death Gratuity 4/10 10-06
- Page 99 and 100:
. Claimant. The claimant is respons
- Page 101 and 102:
2-0700-6 Adjudication 6. Adjudicati
- Page 103 and 104:
(3) If the parties lived apart for
- Page 105 and 106:
(3) If the child does not begin pos
- Page 107 and 108:
Compensation was terminated effecti
- Page 109 and 110:
. Dependency Criteria. The test of
- Page 111 and 112:
(3) Proof of physical or mental inc
- Page 113 and 114:
The CE should prepare a memorandum
- Page 115 and 116:
. Employee Status. The $200 payment
- Page 117 and 118:
(b) Form CA-1617 should be released
- Page 119 and 120:
2-0700-20 Gratuity 20. Gratuity fro
- Page 121 and 122:
2-0700 Exhibit 1: Percentages of En
- Page 123 and 124:
2-0800-2 Definitions 2. Definitions
- Page 125 and 126:
. Employing Agency. The FECA requir
- Page 127 and 128:
claimant, the CE should send a copy
- Page 129 and 130:
(3) The case must be coded as withd
- Page 131 and 132:
entire group of cases must be adjud
- Page 133 and 134:
2-0800-10 Investigation 10. Investi
- Page 135 and 136:
2-0800-13 Affirmative Defense 13. A
- Page 137 and 138:
2-0801 TIME TABLE OF CONTENTS Parag
- Page 139 and 140:
5 U.S.C. 8122 on the ground that no
- Page 141 and 142:
(4) If a claim is not received by O
- Page 143 and 144:
(1) Disappearance During a Period o
- Page 145 and 146:
2-0802 CIVIL EMPLOYEE TABLE OF CONT
- Page 147 and 148:
2-0802-1 Purpose and Scope 1. Purpo
- Page 149 and 150:
(1) The precise time when the worke
- Page 151 and 152:
2-0802-8 Contract Job Cleaners Used
- Page 153 and 154:
2-0802-13 Volunteer Workers with th
- Page 155 and 156:
(1) Whether, prior to the transfer
- Page 157 and 158:
. The pay rate for compensation pur
- Page 159 and 160:
2-0802-24 U.S. Park Police and Secr
- Page 161 and 162:
a participant or crew leader servin
- Page 163 and 164:
2-0803 FACT OF INJURY TABLE OF CONT
- Page 165 and 166:
2-0803-4 Development of Factual Evi
- Page 167 and 168:
2-0804 PERFORMANCE OF DUTY TABLE OF
- Page 169 and 170:
time before or after the end of the
- Page 171 and 172:
(a) A diagram showing the boundarie
- Page 173 and 174:
d. Workers in a Travel Status. (1)
- Page 175 and 176:
2-0804-6 To and From Work 6. To and
- Page 177 and 178:
(a) The reason the employee was req
- Page 179 and 180:
(1) At the time of the injury, the
- Page 181 and 182:
(1) Martha G. List, 26 ECAB 200. Em
- Page 183 and 184:
duty, the CE may approve the case.
- Page 185 and 186:
action taken; and (4) Statements fr
- Page 187 and 188:
2-0804-14 Statutory Exclusions 14.
- Page 189 and 190:
would justify such disobedience. (c
- Page 191 and 192:
(2) The official superior should al
- Page 193 and 194:
c. Development. (1) It is the CE's
- Page 195 and 196:
such as soliciting new members or c
- Page 197 and 198:
c. Performance Ratings. The Board r
- Page 199 and 200:
Where an employee asserts that emot
- Page 201 and 202:
The Board noted that Cannon was unl
- Page 203 and 204:
Since both cases involve procedures
- Page 205 and 206:
Ashberry's disability was not compe
- Page 207 and 208:
no longer be considered so in light
- Page 209 and 210:
2-0804-18 Employing Agency Physical
- Page 211 and 212:
f. This matter was initially addres
- Page 213 and 214:
compensation would be payable for t
- Page 215 and 216:
limited to the period of work-relat
- Page 217 and 218:
(6) Certain other kinds of cases re
- Page 219 and 220:
(2) A nurse becomes disabled by pul
- Page 221 and 222:
the body originally injured is term
- Page 223 and 224:
2-0806 OCCUPATIONAL ILLNESS TABLE O
- Page 225 and 226:
2-0806-1 Purpose and Scope 1. Purpo
- Page 227 and 228:
the following steps, depending on w
- Page 229 and 230:
(4) Exposure to and Identification
- Page 231 and 232:
While records of past medical treat
- Page 233 and 234:
the medical connection between lift
- Page 235 and 236:
(b) The medical evidence presented
- Page 237 and 238:
2-080 Exhibit 2: Sample Letter to C
- Page 239 and 240:
2-0806 Exhibit 3: Sample Letter to
- Page 241 and 242:
TITLE _____________________________
- Page 243 and 244:
2-0806 Exhibit 4: Sample Letter to
- Page 245 and 246:
eason, you should call or write to
- Page 247 and 248:
2-0806 Exhibit 5: Sample Letter to
- Page 249 and 250:
9. [FREE FLOW IF DESIRED] We may wr
- Page 251 and 252:
2-0806 Exhibit 8: Sample Letter to
- Page 253 and 254:
2-0806 Exhibit 9: Sample Letter to
- Page 255 and 256:
If you do not understand any part o
- Page 257 and 258:
2-0806 Exhibit 12: Sample Letter to
- Page 259 and 260:
2-0806 Exhibit 13: Sample Letter to
- Page 261 and 262:
stressful situations in your person
- Page 263 and 264:
TITLE FECA-PT2 Printed: 06/08/2010
- Page 265 and 266:
I am writing in reference to your c
- Page 267 and 268:
2-0806 Exhibit 17: Sample Letter to
- Page 269 and 270:
We may write directly to a physicia
- Page 271 and 272:
2-0806 Exhibit 20: Sample Questions
- Page 273 and 274:
TA Amputation TB Back strain TC Con
- Page 275 and 276:
(D )Other Disability, Occupational
- Page 277 and 278:
a. Traumatic Injury. If an air traf
- Page 279 and 280:
2-0807-6 Period of Entitlement 6. P
- Page 281 and 282:
d. Return to Duty. The injured empl
- Page 283 and 284:
f. The injury was not reported on a
- Page 285 and 286:
W = Total number weeks worked P/W =
- Page 287 and 288:
COP is paid for the entire period o
- Page 289 and 290:
(c) When the physician's report ind
- Page 291 and 292:
(a) Assign or detail the employee t
- Page 293 and 294:
. Monitoring the Claim. (1) If Form
- Page 295 and 296:
(4) If conflicting information appe
- Page 297 and 298:
a. Permanent Total Disability (PTD)
- Page 299 and 300:
(1) Prior to December 7, 1940. No p
- Page 301 and 302:
(2) Impairment due to amputation is
- Page 303 and 304:
. Claims for Increased Schedule Awa
- Page 305 and 306:
compensation for temporary total di
- Page 307 and 308:
Medical. 2-0809-2 Introduction 2. I
- Page 309 and 310:
CE is ready to evaluate the evidenc
- Page 311 and 312:
the physician with a complete pictu
- Page 313 and 314:
(3) Personal habits such as smoking
- Page 315 and 316: games or operating a construction b
- Page 317 and 318: Jane Doe, date of birth 04/06/1965,
- Page 319 and 320: elated to the employee’s duties;
- Page 321 and 322: 16. Physical Therapy 04/01 01-06 03
- Page 323 and 324: evaluating the merits of medical re
- Page 325 and 326: situation where ten days earlier th
- Page 327 and 328: each opinion. The value of the evid
- Page 329 and 330: manipulation of the body. They incl
- Page 331 and 332: . The DMA's performance of these fu
- Page 333 and 334: evidence from physicians who have n
- Page 335 and 336: e. In cases involving a preexisting
- Page 337 and 338: (1) The consultant should be asked
- Page 339 and 340: value). Based on the results of thi
- Page 341 and 342: However, if the impartial specialis
- Page 343 and 344: 2-0810-13 Exclusion of Medical Evid
- Page 345 and 346: Leanna Garlington, 37 ECAB 849). Re
- Page 347 and 348: (d) A suggested supplier, if any. (
- Page 349 and 350: need for further treatment as detai
- Page 351 and 352: 2-0810-18 Transfer of Medical Care
- Page 353 and 354: 2-0810 Exhibit 1: Information from
- Page 355 and 356: Dear CLAIMANT NAME: We need the fol
- Page 357 and 358: 2-0810 Exhibit 3: General Guideline
- Page 359 and 360: 2-0810 Exhibit 5: Sample Paragraph
- Page 361 and 362: 2-0810 Exhibit 7: Letter of Warning
- Page 363 and 364: In addition, a primary goal of case
- Page 365: (3) Release Form CA-1008 and Pamphl
- Page 369 and 370: f. If the evidence obtained as a re
- Page 371 and 372: eligible for disability benefits. A
- Page 373 and 374: f. Physician's estimate of the date
- Page 375 and 376: 2-0812 PERIODIC REVIEW OF DISABILIT
- Page 377 and 378: 2-0812-1 Purpose and Scope 1. Purpo
- Page 379 and 380: determine the status of dependents
- Page 381 and 382: whether disability is related to th
- Page 383 and 384: earnings or activity is in question
- Page 385 and 386: eferred to the Office of Inspector
- Page 387 and 388: . Suspension of Compensation. OWCP
- Page 389 and 390: certification clauses on the CA-103
- Page 391 and 392: SI Payment/Entitlement Suspension i
- Page 393 and 394: with the return to work effort. CFF
- Page 395 and 396: should be placed in a PN status. OP
- Page 397 and 398: force. 10. If the business has had
- Page 399 and 400: I am writing in follow up to the Fo
- Page 401 and 402: 2-0812 Exhibit 6 - Periodic Entitle
- Page 403 and 404: Service. On 03/14/2003, the claiman
- Page 405 and 406: Authorized Medical Care for Substan
- Page 407 and 408: a. OPM's regulations on retention r
- Page 409 and 410: d. To identify cases for early inte
- Page 411 and 412: 2-0813-7 Communication Among the CE
- Page 413 and 414: d. Cooperative Agreement. The title
- Page 415 and 416: ehabilitation process. 2-0813-11 Fa
- Page 417 and 418:
(2) To reduce compensation in this
- Page 419 and 420:
The specificity of the reasons offe
- Page 421 and 422:
in conjunction with graded conditio
- Page 423 and 424:
(1) Where the claimant cannot perfo
- Page 425 and 426:
2-0813 Exhibit 2: Non-Cooperation W
- Page 427 and 428:
2-0813 Exhibit 4: Sample Letter to
- Page 429 and 430:
2-0814 REEMPLOYMENT: DETERMINING WA
- Page 431 and 432:
Exhibits 1. Sample Letter to Claima
- Page 433 and 434:
. Preliminary Assessment of Positio
- Page 435 and 436:
(b) If the attending physician cont
- Page 437 and 438:
(3) The employing agency will be as
- Page 439 and 440:
e. Payment/Reimbursement of Relocat
- Page 441 and 442:
have no appeal rights attached. c.
- Page 443 and 444:
were not reported to OWCP or were o
- Page 445 and 446:
(3) If the employee can work only p
- Page 447 and 448:
this instance the CE will need to e
- Page 449 and 450:
d. Unacceptable Reasons for Abandon
- Page 451 and 452:
closure of an installation, cessati
- Page 453 and 454:
Code, and returns to duty under ret
- Page 455 and 456:
If you receive an increase in pay o
- Page 457 and 458:
2-0814 Exhibit 3: Sample Letter To
- Page 459 and 460:
RATE DATE FOR SCHEDULE AWARDS 01/10
- Page 461 and 462:
(1) Kinds of Appointments. The Post
- Page 463 and 464:
year, in the teaching profession, w
- Page 465 and 466:
(b) Census enumerators; (c) Casual
- Page 467 and 468:
The CE should consider these factor
- Page 469 and 470:
The greatest of these pay rates wil
- Page 471 and 472:
the Department of Veterans Affairs
- Page 473 and 474:
degree of expense, hardship, and in
- Page 475 and 476:
(2) Basic bi-weekly pay x premium p
- Page 477 and 478:
2-0900-9 Computing Daily Pay Rate 9
- Page 479 and 480:
2-0900-11 Computing Monthly Pay Rat
- Page 481 and 482:
The salary for these employees may
- Page 483 and 484:
2-0901 COMPUTING COMPENSATION TABLE
- Page 485 and 486:
2-0901-2 Related Topics 2. Related
- Page 487 and 488:
(4) A GS-12 CE or designated CE may
- Page 489 and 490:
2-0901-4 Factors in Computing Compe
- Page 491 and 492:
(3) For schedule award payments, th
- Page 493 and 494:
(4) Compensation payable for less t
- Page 495 and 496:
2-0901-9 Special Determinations 9.
- Page 497 and 498:
2-0901-11 Maximum Compensation 11.
- Page 499 and 500:
payment. a. Beginning Date. Schedul
- Page 501 and 502:
(3) ( ) (a) is capable of earning (
- Page 503 and 504:
automatic pay increases. For exampl
- Page 505 and 506:
claimant to a higher pay rate under
- Page 507 and 508:
(a) the beneficiary's maintenance,
- Page 509 and 510:
Letter CA-1208 to the claimant, wit
- Page 511 and 512:
01/01/76 4.4 10/10/76 18.96-28.44 9
- Page 513 and 514:
01/02/2000 44.98-67.47 224.91-337.3
- Page 515 and 516:
10/07/79 144.56 722.78 - (2,891.12)
- Page 517 and 518:
*Calendar Days 01/01/2001 3.3 365 1
- Page 519 and 520:
PERCENTAGE TABLE OF SCHEDULE AWARDS
- Page 521 and 522:
2-0901 Exhibit 6: Activity Codes AC
- Page 523 and 524:
12. Tennessee Valley Authority 02/9
- Page 525 and 526:
. Death Benefits. When compensation
- Page 527 and 528:
(3) Certification. The CE should ha
- Page 529 and 530:
elected, refer the case to the inac
- Page 531 and 532:
(b) If there is accrued compensatio
- Page 533 and 534:
Centers, and DVA Hospitals. If the
- Page 535 and 536:
(b) The claimant may be entitled to
- Page 537 and 538:
d. Obtaining Elections--Educational
- Page 539 and 540:
(3) The CE must advise the claimant
- Page 541 and 542:
c. Injuries On and After September
- Page 543 and 544:
Based on information contained in t
- Page 545 and 546:
2-1000-16 Benefits for Judicial Off
- Page 547 and 548:
(a) Calculate the number of weeks w
- Page 549 and 550:
I. Claimants must elect between Fed
- Page 551 and 552:
2-1000 Exhibit 2: OPM Contact List
- Page 553 and 554:
When a third party is or may be leg
- Page 555 and 556:
(6) Ltr. CA-1109, Authorization to
- Page 557 and 558:
7. Administration of Third Party Ca
- Page 559 and 560:
(3) If not accurate or complete, th
- Page 561 and 562:
the DCE, is urgent should be sent i
- Page 563 and 564:
(3) Provide the claimant or attorne
- Page 565 and 566:
for a course of action. All formal
- Page 567 and 568:
In any other case, where a judgment
- Page 569 and 570:
(b) 5 percent of the total to be al
- Page 571 and 572:
To determine the amount to be liste
- Page 573 and 574:
(6) Section 8133(a) of the FECA pro
- Page 575 and 576:
(2) The initial demand letter in an
- Page 577 and 578:
of the employee. The USPS cannot re
- Page 579 and 580:
not be referred to the FEEWC until
- Page 581 and 582:
FECA-PT2 Printed: 06/08/2010 581
- Page 583 and 584:
a. Under 5 U.S.C. § 8127(b) and in
- Page 585 and 586:
. Should an application be submitte
- Page 587 and 588:
and the requested fee is reduced du
- Page 589 and 590:
2-1200 Exhibit 1: Sample Formal Dec
- Page 591 and 592:
2-1300 LUMP SUM PAYMENTS TABLE OF C
- Page 593 and 594:
2-1300-3 Requests for Lump-Sum Paym
- Page 595 and 596:
2-1300-4 Calculating Lump-Sum Sched
- Page 597 and 598:
2-1300 Exhibit 2: Sample Appealable
- Page 599 and 600:
3. REVIEW BY THE EMPLOYEES' COMPENS
- Page 601 and 602:
SIGNATURE _________________________
- Page 603 and 604:
We have received your request for a
- Page 605 and 606:
2-1400 DISALLOWANCES TABLE OF CONTE
- Page 607 and 608:
2-1400-1 Purpose and Scope Purpose
- Page 609 and 610:
a. Initial Disallowances. Such disa
- Page 611 and 612:
(1) Failure to Appear for Medical A
- Page 613 and 614:
(1) The name and location of the em
- Page 615 and 616:
injury caused no disability for wor
- Page 617 and 618:
(3) A specific service which the cl
- Page 619 and 620:
2-1400-7 How to Issue Pre-Terminati
- Page 621 and 622:
(a) The case is being referred beca
- Page 623 and 624:
(a) Compensation is being terminate
- Page 625 and 626:
. Source of Advice. District office
- Page 627 and 628:
usual rate, i.e., 75 percent of the
- Page 629 and 630:
objective findings to support your
- Page 631 and 632:
2-1400 Exhibit 3: Sample Notice of
- Page 633 and 634:
2-1400 Exhibit 4: Sample Letter Con
- Page 635 and 636:
2-1400 Exhibit 6: Sample Notice of
- Page 637 and 638:
2-1400 Exhibit 8: Sample Letter Con
- Page 639 and 640:
2-1400 Exhibit 10: Sample Letter De
- Page 641 and 642:
2-1500 RECURRENCES TABLE OF CONTENT
- Page 643 and 644:
(d) Closure of a base or other faci
- Page 645 and 646:
(1) The medical evidence needed to
- Page 647 and 648:
c. Case Management. The CE should c
- Page 649 and 650:
emains the same regardless of wheth
- Page 651 and 652:
2-1600 REVIEW PROCESS TABLE OF CONT
- Page 653 and 654:
c. Formal Decision. Chapter 2-1400
- Page 655 and 656:
FECA-PT2 Printed: 06/08/2010 655
- Page 657 and 658:
the request. H&R will acknowledge r
- Page 659 and 660:
spouse or child prevents his or her
- Page 661 and 662:
OWCP shall pay fees requested by wi
- Page 663 and 664:
2-1601-9 Cases Returned from H&R 9.
- Page 665 and 666:
2-1601 Exhibit 2: Sample Letters Ac
- Page 667 and 668:
Exhibit 3, page 1 of 3: Hearing Not
- Page 669 and 670:
Exhibit 3, page 3 of 3: Hearing Ins
- Page 671 and 672:
2-1601 Exhibit 5: Request for Comme
- Page 673 and 674:
2-1602 RECONSIDERATIONS TABLE OF CO
- Page 675 and 676:
2-1602-2 Policy 2. Policy. The foll
- Page 677 and 678:
d. Decision. An untimely applicatio
- Page 679 and 680:
percentage of the award under the S
- Page 681 and 682:
(2) The cover letter to the agency
- Page 683 and 684:
2-1602 Exhibit 1: Sample Letter Ret
- Page 685 and 686:
Dear CLAIMANT NAME: We have reviewe
- Page 687 and 688:
2-1602 Exhibit 5: Sample Compensati
- Page 689 and 690:
2-1603 APPEALS TABLE OF CONTENTS Pa
- Page 691 and 692:
d. Timeliness of Filing. A person r
- Page 693 and 694:
2-1603-6 Cases Returned to District
- Page 695 and 696:
2-1700 SPECIAL ACT CASES TABLE OF C
- Page 697 and 698:
2-1700-4 Peace Corps 4. Peace Corps
- Page 699 and 700:
(2) Staff Spouses. (a) The spouses
- Page 701 and 702:
Compensation for loss of wages may
- Page 703 and 704:
(3) Return from Service Abroad. d.
- Page 705 and 706:
Section 5 U.S.C. 8101(4), which pro
- Page 707 and 708:
(1)While at a Job Corps Center, an
- Page 709 and 710:
(1)Enrollees are required to report
- Page 711 and 712:
coverage under 5 U.S.C. 8101. b. Co
- Page 713 and 714:
FECA-PT2 Printed: 06/08/2010 713
- Page 715 and 716:
2-1800-2 Authority 2. Authority. Ho
- Page 717 and 718:
determined by the type of vehicle,
- Page 719 and 720:
greatest current fair market value
- Page 721 and 722:
Such certification from an architec
- Page 723 and 724:
over $10,000, and that amount must
- Page 725 and 726:
2-1800-7 Housing Modifications for
- Page 727 and 728:
send an approval letter along with
- Page 729 and 730:
By signing this agreement, all part
- Page 731 and 732:
By signing this agreement, all part
- Page 733 and 734:
Memorandum of Agreement - Modificat
- Page 735 and 736:
Memorandum of Agreement - Housing M