- Page 1 and 2:
AGREEMENT between MINNESOTA STATE E
- Page 3 and 4:
Section 5 - Liquidation ...........
- Page 5 and 6:
Section 7 - Filling Positions .....
- Page 7 and 8:
ARTICLE 19 - INSURANCE ............
- Page 9 and 10:
C. Union Notification..............
- Page 11 and 12:
4. Part-Time/Unscheduled Employees
- Page 13 and 14:
Minnesota State Lottery ...........
- Page 15 and 16:
9. LCR 1 Seniority ................
- Page 17 and 18:
ARTICLE 1 - PREAMBLE This Agreement
- Page 19 and 20:
3. Trainee and Provisional Appointm
- Page 21 and 22:
E. Rest Periods. All employees shal
- Page 23 and 24:
B. Additional Hours. When the Appoi
- Page 25 and 26:
D. Compensatory Time Liquidation in
- Page 27 and 28:
Section 2. Observed Holidays. A. Fi
- Page 29 and 30:
Section 8. Work on a Holiday. A. Sc
- Page 31 and 32:
Employees on a military leave under
- Page 33 and 34: Section 2. Sick Leave Accrual. All
- Page 35 and 36: Section 6. Transfer to Another Appo
- Page 37 and 38: L. Paid Administrative Leave. At th
- Page 39 and 40: Section 6. Reinstatement after Leav
- Page 41 and 42: F. Any pregnant employee assigned t
- Page 43 and 44: 4. Emergency employee. "Emergency e
- Page 45 and 46: A. Bidding. Selection of employees
- Page 47 and 48: Section 8. Effects of Changes in Po
- Page 49 and 50: For probationary periods that begin
- Page 51 and 52: B. Advance Notice. In the event a p
- Page 53 and 54: d. Bump Within Thirty-Five (35) Mil
- Page 55 and 56: 5. When a vacancy exists in a class
- Page 57 and 58: 1. Recall to a permanent position f
- Page 59 and 60: In order to be eligible for emergen
- Page 61 and 62: If the Appointing Authority has rea
- Page 63 and 64: Section 8. Resignations. An employe
- Page 65 and 66: Section 5. Arbitrator's Authority.
- Page 67 and 68: D. Compensation Grids 2A and 3A. Em
- Page 69 and 70: Employees who separate from State s
- Page 71 and 72: All insurance eligible employees wi
- Page 73 and 74: 4. Disabled Child. A disabled depen
- Page 75 and 76: However, notwithstanding the paragr
- Page 77 and 78: E. Maintaining Eligibility for Empl
- Page 79 and 80: The request to change coverage must
- Page 81 and 82: D. Open Enrollment. 1. Frequency an
- Page 83: 2014-2015 Benefit Provision Emergen
- Page 87 and 88: . If no agreement is reached within
- Page 89 and 90: Employee’s Annual Base Salary Gro
- Page 91 and 92: 3. Children/Grandchildren. An emplo
- Page 93 and 94: Section 2. Automobile Expense. When
- Page 95 and 96: Section 6. Special Expenses. When p
- Page 97 and 98: Section 2. Covered Expenses. Employ
- Page 99 and 100: ARTICLE 25 - UNION RIGHTS Section 1
- Page 101 and 102: ARTICLE 29 - LEGISLATIVE RATIFICATI
- Page 103 and 104: D. Parking Committee. The Committee
- Page 105 and 106: ARTICLE 33 - EMPLOYEE ASSISTANCE PR
- Page 107 and 108: FOR THE UNION FOR THE EMPLOYER ____
- Page 109 and 110: TECHNICAL UNIT UNIT 7 Case No: 80-P
- Page 111 and 112: Table 2: For pay periods containing
- Page 113 and 114: APPENDIX C - VACATION Eligible empl
- Page 115 and 116: APPENDIX E-1 Compensation Grid 2 Un
- Page 117 and 118: APPENDIX E-1 Compensation Grid 3 Un
- Page 119 and 120: APPENDIX E-1 Compensation Grid 3 (c
- Page 121 and 122: APPENDIX E-1 Compensation Grid 4/Co
- Page 123 and 124: APPENDIX E-1 Compensation Grid 4/Co
- Page 125 and 126: APPENDIX E-1 Compensation Grid 7 Un
- Page 127 and 128: APPENDIX E-1 Compensation Grid 7 (c
- Page 129 and 130: Transportation Associate APPENDIX E
- Page 131 and 132: Building Maintenance Coordinator AP
- Page 133 and 134: APPENDIX E-2 Compensation Grid 3 (c
- Page 135 and 136:
Laborer - General APPENDIX E-2 Comp
- Page 137 and 138:
APPENDIX E-2 Compensation Grid 4/Co
- Page 139 and 140:
Human Services Technician APPENDIX
- Page 141 and 142:
APPENDIX E-2 Compensation Grid 7 (c
- Page 143 and 144:
APPENDIX E-2 Compensation Grid 7C U
- Page 145 and 146:
2013-2015 AFSCME Contract - Page 12
- Page 147 and 148:
7/1/2013 - 6/30/2014 7/1/2014 - 6/3
- Page 149 and 150:
7/1/2013 - 6/30/2014 7/1/2014 - 6/3
- Page 151 and 152:
Snow grooming machine with hydrauli
- Page 153 and 154:
Human Services, Department of - Wil
- Page 155 and 156:
APPENDIX H - CLASS OPTIONS A "class
- Page 157 and 158:
College Laboratory Assistant 2 Acco
- Page 159 and 160:
Human Services Technician Law Compl
- Page 161 and 162:
APPENDIX I The following Junior/Sen
- Page 163 and 164:
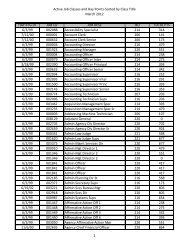
APPENDIX K - APPOINTING AUTHORITY/D
- Page 165 and 166:
The Labor Relations Bureau encourag
- Page 167 and 168:
Adjustable platforms for terminals
- Page 169 and 170:
APPENDIX N The following is a link
- Page 171 and 172:
June 27, 2013 Page 2 2. Since job t
- Page 173 and 174:
200 Centennial Office Building 658
- Page 175 and 176:
200 Centennial Office Building 658
- Page 177 and 178:
200 Centennial Office Building 658
- Page 179 and 180:
200 Centennial Office Building 658
- Page 181 and 182:
200 Centennial Office Building 658
- Page 183 and 184:
April 22, 2009 Eliot Seide, Executi
- Page 185 and 186:
June 26, 2013 Jo Pels, State Field
- Page 187 and 188:
DATE: July 2, 2013 TO: FROM: RE: St
- Page 189 and 190:
APPENDIX P - UNIT 6 POSITION QUALIF
- Page 191 and 192:
Class Specifications (Specs) - Minn
- Page 193 and 194:
Promotion - The upward movement of
- Page 195 and 196:
APPENDIX R - DRUG TESTING 1. INTROD
- Page 197 and 198:
3. The right to access information
- Page 199 and 200:
APPENDIX T - SUPPLEMENTAL AGREEMENT
- Page 201 and 202:
4. In the event of a need for plann
- Page 203 and 204:
Employees may be permitted to adjus
- Page 205 and 206:
DEPARTMENT OF AGRICULTURE Article 1
- Page 207 and 208:
It is further understood that the D
- Page 209 and 210:
Section 1. Definition. "Work Statio
- Page 211 and 212:
DEPARTMENT OF CORRECTIONS ALL SENIO
- Page 213 and 214:
Article 6 Wages Article 18 of the M
- Page 215 and 216:
In the event, the notice of overtim
- Page 217 and 218:
Filling Positions Vacated by Layoff
- Page 219 and 220:
Workforce Development Disability De
- Page 221 and 222:
Small Business Development Center N
- Page 223 and 224:
12. An employee who does not make a
- Page 225 and 226:
In the event all capable employees
- Page 227 and 228:
use of an intermittent employee; us
- Page 229 and 230:
GAMBLING CONTROL BOARD Article 1 Fl
- Page 231 and 232:
An employee who refuses a job and t
- Page 233 and 234:
1) job and retraining opportunities
- Page 235 and 236:
7. The Department shall supply the
- Page 237 and 238:
An employee selecting this option s
- Page 239 and 240:
Article 2 Probation Article 12, Sec
- Page 241 and 242:
Shifts Between Days Off (For all em
- Page 243 and 244:
There are several reasons that Mana
- Page 245 and 246:
There are several reasons Managemen
- Page 247 and 248:
2. No more than seven (7) consecuti
- Page 249 and 250:
If you work the night shift, your s
- Page 251 and 252:
Variable schedule employees will be
- Page 253 and 254:
5. Have the right to assign mandato
- Page 255 and 256:
On-Call Assignments. Article 6, Sec
- Page 257 and 258:
This provision does not diminish yo
- Page 259 and 260:
(For Anoka Region only) The campus
- Page 261 and 262:
DEPARTMENT OF HUMAN SERVICES/STATE
- Page 263 and 264:
g) No more than ten (10) workdays i
- Page 265 and 266:
The sign-up procedure for voluntary
- Page 267 and 268:
Variable schedule employees will be
- Page 269 and 270:
3. Offer the overtime to capable em
- Page 271 and 272:
Vacation Vacation Leave Article 8,
- Page 273 and 274:
Hours of Work Schedule Posting: Art
- Page 275 and 276:
Work Period: Your supervisor may te
- Page 277 and 278:
Union Meetings: Management will mak
- Page 279 and 280:
METO Snow Removal Management will c
- Page 281 and 282:
Work on a Holiday: Article 7, Secti
- Page 283 and 284:
Job Posting Article 12, Section 5 o
- Page 285 and 286:
The Appointing Authority agrees to
- Page 287 and 288:
4. Nine (9) consecutive hours of wo
- Page 289 and 290:
8. DLI will extend the posting peri
- Page 291 and 292:
Section 3. Review of Requests. Mana
- Page 293 and 294:
Article 3 Vacation Accrual - Duluth
- Page 295 and 296:
Appendix D of the Master Agreement
- Page 297 and 298:
Article 7 Shift Differential Articl
- Page 299 and 300:
MN.IT SERVICES Article 1 Hours of W
- Page 301 and 302:
Article 4 Vacation Leave Article 8,
- Page 303 and 304:
Full-time unlimited and seasonal, a
- Page 305 and 306:
13. Conflicts. The following practi
- Page 307 and 308:
25. Balloon Payments for Summer Ins
- Page 309 and 310:
39. Vacancies. Article 12, Section
- Page 311 and 312:
51. Life Insurance. The employer wi
- Page 313 and 314:
DEPARTMENT OF NATURAL RESOURCES Art
- Page 315 and 316:
Article 4 Rate of Pay The provision
- Page 317 and 318:
Article 10 Pay Differentials A. Sel
- Page 319 and 320:
Employees hired into these classifi
- Page 321 and 322:
MINNESOTA POLLUTION CONTROL AGENCY
- Page 323 and 324:
Article 3 On-Call Upon mutual agree
- Page 325 and 326:
C. Holidays and Paid Leave Hours. E
- Page 327 and 328:
The employee shall have the right t
- Page 329 and 330:
Section 2 Benefits A. Eligibility.
- Page 331 and 332:
If a position in a principal place
- Page 333 and 334:
Section 4 Filling of Seasonal Vacan
- Page 335 and 336:
Section 9 Waiver of Notice for Shif
- Page 337 and 338:
The immediate supervisor shall dete
- Page 339 and 340:
This group shall be comprised of up
- Page 341 and 342:
It is specifically understood by th
- Page 343 and 344:
Article 7 Tools and Equipment Loss
- Page 345 and 346:
Article 12 Probationary Period The
- Page 347 and 348:
Post the vacant position at the pre
- Page 349 and 350:
July 30, 2001 Bob Hilliker Business
- Page 351 and 352:
Proposal for Transportation Special
- Page 353 and 354:
Project Steps & Time Frame: ACTION
- Page 355 and 356:
Article 3 Overtime All overtime sha
- Page 357 and 358:
f. Emergency situations. To no long
- Page 359 and 360:
Article 7 Uniforms Employees servin
- Page 361 and 362:
To no longer be permanently assigne
- Page 363 and 364:
The Administrator shall make every
- Page 365 and 366:
For this subsection only, a schedul
- Page 367 and 368:
2. Distribution of overtime work fo
- Page 369 and 370:
Article 9 Overnight Activities The
- Page 371 and 372:
No employee shall be assigned an ex
- Page 373:
Article 5 Additional Shifts Of Work