De l'innovation au changement - Gouvernement du Québec
De l'innovation au changement - Gouvernement du Québec
De l'innovation au changement - Gouvernement du Québec
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
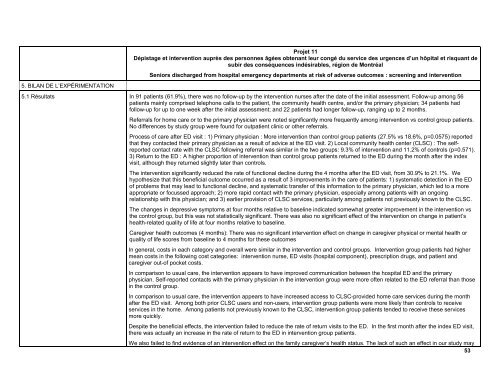
5. BILAN DE L’EXPÉRIMENTATION<br />
Projet 11<br />
Dépistage et intervention <strong>au</strong>près des personnes âgées obtenant leur congé <strong>du</strong> service des urgences d’un hôpital et risquant de<br />
subir des conséquences indésirables, région de Montréal<br />
Seniors discharged from hospital emergency departments at risk of adverse outcomes : screening and intervention<br />
5.1 Résultats In 91 patients (61.9%), there was no follow-up by the intervention nurses after the date of the initial assessment. Follow-up among 56<br />
patients mainly comprised telephone calls to the patient, the community health centre, and/or the primary physician; 34 patients had<br />
follow-up for up to one week after the initial assessment; and 22 patients had longer follow-up, ranging up to 2 months.<br />
Referrals for home care or to the primary physician were noted significantly more frequently among intervention vs control group patients.<br />
No differences by study group were found for outpatient clinic or other referrals.<br />
Process of care after ED visit : 1) Primary physician : More intervention than control group patients (27.5% vs 18.6%, p=0.0575) reported<br />
that they contacted their primary physician as a result of advice at the ED visit. 2) Local community health center (CLSC) : The selfreported<br />
contact rate with the CLSC following referral was similar in the two groups: 9.3% of intervention and 11.2% of controls (p=0.571).<br />
3) Return to the ED : A higher proportion of intervention than control group patients returned to the ED <strong>du</strong>ring the month after the index<br />
visit, although they returned slightly later than controls.<br />
The intervention significantly re<strong>du</strong>ced the rate of functional decline <strong>du</strong>ring the 4 months after the ED visit, from 30.9% to 21.1%. We<br />
hypothesize that this beneficial outcome occurred as a result of 3 improvements in the care of patients: 1) systematic detection in the ED<br />
of problems that may lead to functional decline, and systematic transfer of this information to the primary physician, which led to a more<br />
appropriate or focussed approach; 2) more rapid contact with the primary physician, especially among patients with an ongoing<br />
relationship with this physician; and 3) earlier provision of CLSC services, particularly among patients not previously known to the CLSC.<br />
The changes in depressive symptoms at four months relative to baseline indicated somewhat greater improvement in the intervention vs<br />
the control group, but this was not statistically significant. There was also no significant effect of the intervention on change in patient’s<br />
health-related quality of life at four months relative to baseline.<br />
Caregiver health outcomes (4 months): There was no significant intervention effect on change in caregiver physical or mental health or<br />
quality of life scores from baseline to 4 months for these outcomes<br />
In general, costs in each category and overall were similar in the intervention and control groups. Intervention group patients had higher<br />
mean costs in the following cost categories: intervention nurse, ED visits (hospital component), prescription drugs, and patient and<br />
caregiver out-of pocket costs.<br />
In comparison to usual care, the intervention appears to have improved communication between the hospital ED and the primary<br />
physician. Self-reported contacts with the primary physician in the intervention group were more often related to the ED referral than those<br />
in the control group.<br />
In comparison to usual care, the intervention appears to have increased access to CLSC-provided home care services <strong>du</strong>ring the month<br />
after the ED visit. Among both prior CLSC users and non-users, intervention group patients were more likely than controls to receive<br />
services in the home. Among patients not previously known to the CLSC, intervention group patients tended to receive these services<br />
more quickly.<br />
<strong>De</strong>spite the beneficial effects, the intervention failed to re<strong>du</strong>ce the rate of return visits to the ED. In the first month after the index ED visit,<br />
there was actually an increase in the rate of return to the ED in intervention group patients.<br />
We also failed to find evidence of an intervention effect on the family caregiver’s health status. The lack of such an effect in our study may<br />
53